Online CDIP Practice TestMore AHIMA Products >
Free AHIMA CDIP Exam Dumps Questions
AHIMA CDIP: Certified Documentation Integrity Practitioner
- Get instant access to CDIP practice exam questions
- Get ready to pass the Certified Documentation Integrity Practitioner exam right now using our AHIMA CDIP exam package, which includes AHIMA CDIP practice test plus an AHIMA CDIP Exam Simulator.
- The best online CDIP exam study material and preparation tool is here.
Question 1
Whether or not queries should be kept as a permanent part of the medical record is decided by
Correct Answer:D
According to the AHIMA/ACDIS Query Practice Brief, whether or not queries should be kept as a permanent part of the medical record is decided by the organizational policy of each facility1. There is no federal or state law that mandates the retention of queries in the medical record, although some external reviewers may request copies of queries to validate the query wording and compliance2. Physician preference is not a valid factor in determining the query retention policy, as queries should be handled consistently across the organization3. Therefore, the correct answer is D. organizational policy. References:
✑ Guidelines for Achieving a Compliant Query Practice (2019 Update) - AHIMA
✑ Q&A: Develop policies regarding query retention | ACDIS
✑ Q&A: Keep query retention policies consistent | ACDIS
Question 2
Which factors are important to include when refocusing the primary vision of a clinical documentation integrity (CDI) program?
Correct Answer:B
A CDI program??s vision should reflect its purpose, values, and goals, and align with the organization??s overall vision and mission. Value and mission statements help define the CDI program??s role, scope, and objectives, and communicate them to stakeholders. Reporting and the use of technology are important tools for a CDI program, but they are not part of its vision. Benchmarks and case mix index are performance indicators that measure the CDI program??s outcomes, but they do not reflect its vision. Diagnostic related groups and revenue cycle are aspects of reimbursement that may be affected by the CDI program, but they are not the primary focus of its vision.
Question 3
The correct coding for insertion of a dialysis catheter into the right internal jugular vein with the tip ending in the cavoatrial junction is
Correct Answer:A
According to the ICD-10-PCS Reference Manual 2023, the insertion of a dialysis catheter into the right internal jugular vein with the tip ending in the cavoatrial junction is coded as follows1:
✑ The first character 0 indicates the Medical and Surgical section.
✑ The second character 5 indicates the Extracorporeal or Systemic Assistance and Performance root operation, which is defined as "Putting in or on a device that completely takes over a body function by extracorporeal means"1.
✑ The third character H indicates the Central Vein body system, which includes the internal jugular vein1.
✑ The fourth character M indicates the Infusion Device device value, which is defined as "A device that is inserted into a body part to deliver fluids or other substances to a body part or into the circulation"1.
✑ The fifth character 3 indicates the Right Internal Jugular Vein body part value, which is the specific site of the procedure1.
✑ The sixth character 3 indicates the Percutaneous approach, which is defined as "Entry, by puncture or minor incision, of instrumentation through the skin or mucous membrane and any other body layers necessary to reach and visualize the site of the procedure"1.
✑ The seventh character Z indicates No Qualifier, which means there is no additional information necessary to complete the code1.
Therefore, the correct coding for insertion of a dialysis catheter into the right internal jugular vein with the tip ending in the cavoatrial junction is 05HM33Z.
References:
✑ ICD-10-PCS Reference Manual 20231
Question 4
The facility has received a clinical validation denial for sepsis. The denial states sepsis is not a clinically valid diagnosis because it does not meet Sepsis-3 criteria. The facility has a policy stating it uses Sepsis-2 criteria. What is the BEST next step?
Correct Answer:D
Question 5
What type of query may NOT be used in circumstances where only clinical indicators of a condition are present, and the condition/diagnosis has not been documented in the health record?
Correct Answer:D
A yes/no query may not be used in circumstances where only clinical indicators of a condition are present, and the condition/diagnosis has not been documented in the health record because it may lead to leading or suggesting a diagnosis that is not supported by the provider??s documentation. A yes/no query should only be used when there is clear and consistent documentation of a condition/diagnosis in the health record, and the query is seeking confirmation or denial of a specific fact or detail related to that condition/diagnosis. A multiple-choice, open-ended, or verbal query may be more appropriate to allow the provider to choose from a list of possible diagnoses, provide additional information, or explain the clinical reasoning behind the documentation. (CDIP Exam Preparation Guide) References:
✑ CDIP Exam Content Outline1
✑ CDIP Exam Preparation Guide2
✑ AHIMA Practice Brief: Guidelines for Achieving a Compliant Query Practice3
Question 6
Based on the flowchart below, at what point might the clinical documentation integrity practitioner (CDIP) enlist the help of the physician advisor/champion?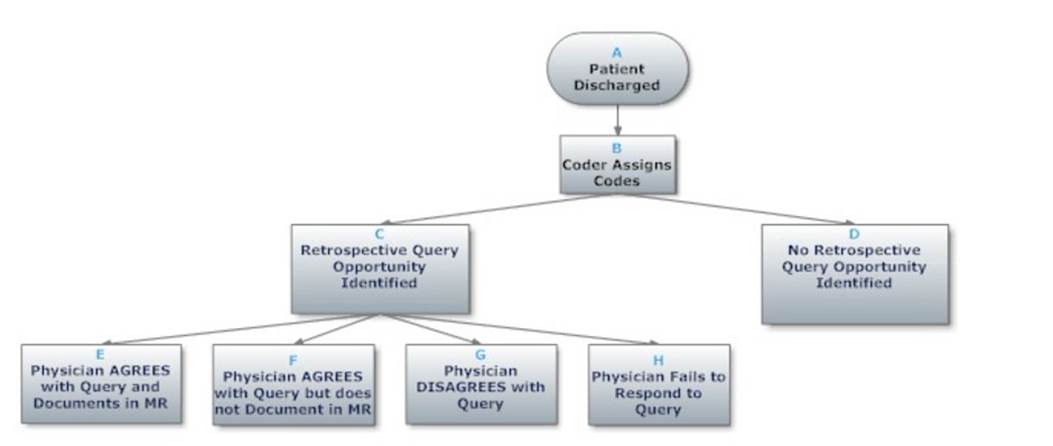
Correct Answer:B